Medical device development
Intracranial Multimodal Sensor for brain diseases
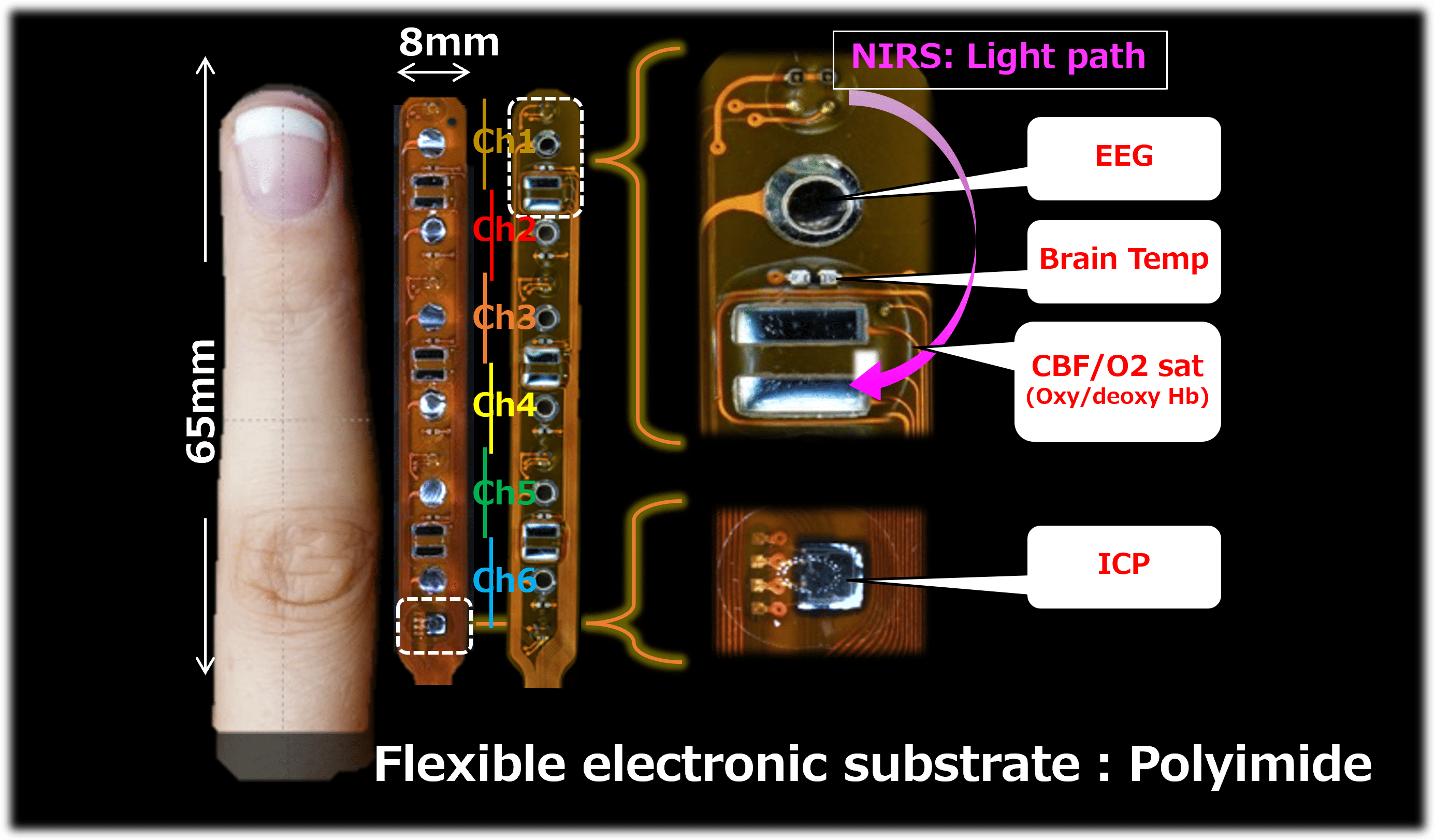
Multimodal Sensor
We are Yamaguchi Univ-based venture established to commercialize innovative diagnostic and treatment methods for severe brain diseases.
By appropriately arranging multiple sensors (brain temperature, EEG, intracranial pressure, NIRS: cerebral blood flow, brain tissue oxygen saturation) on a flexible substrate, we aim to measure various pathological brain activities.
This device, which measures brain activity from multiple angles, will make it possible to monitor the neural activity of patients with severe brain damage (trauma, stroke, epilepsy, post-cardiac arrest hypoxia) 24 hours a day at the bedside.
This system will detect pathologies that do not show up in imaging tests and worsening brain pathologies that do not show up as symptoms, allowing patients to receive treatment promptly.
Brain activity measurement technology
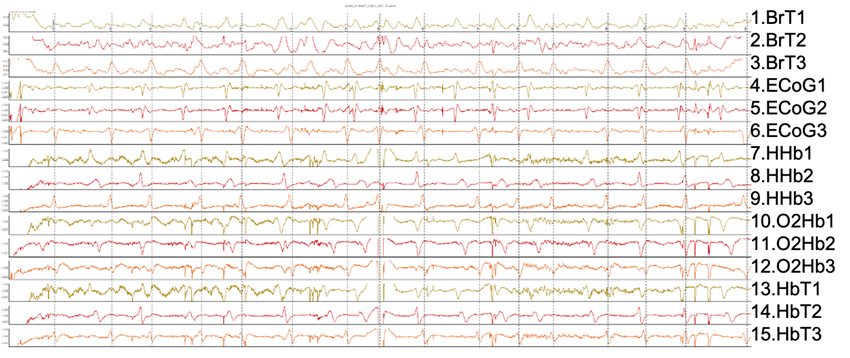
BrT: brain temperature, ECoG: electrocorticogram, HHb: deoxyhemoglobin, O2Hb: oxyhemoglobin, HbT: total hemoglobin
Our brain activity measurement technology measures brain activity using several different sensing technologies, but it is important to detect pathological activity from the obtained signals.
So far, evaluation of abnormal brain activity relies on the expertise of medical professionals based on their experience.
Promising ways to solve this situation include using machine learning to create classifiers from large amounts of data and extracting features based on time-frequency analysis technology.
We aim to use this multifactorial brain activity measurement technology to improve the prognosis of severe brain injuries.
Unmet medical needs
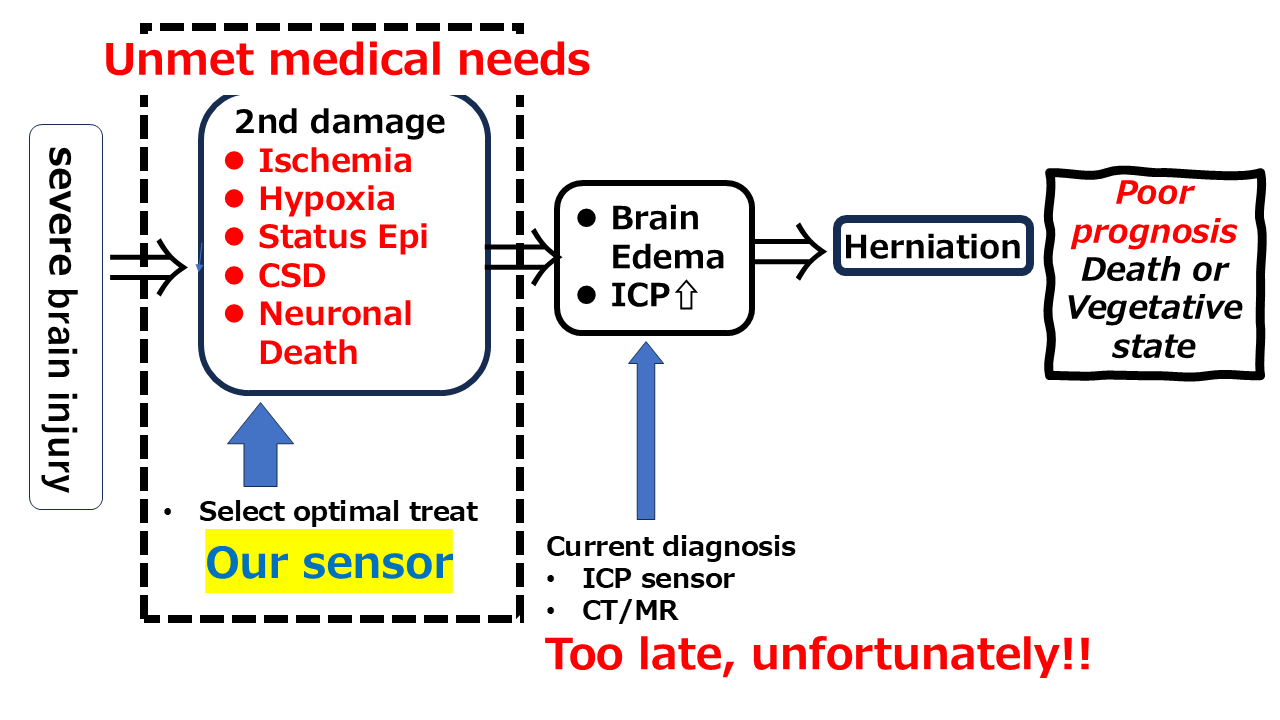
Currently, imaging diagnosis and intracranial pressure (ICP) sensors are the mainstream for diagnosing severe brain injuries, resulting in vague and slow judgments that are like "stroking a blind elephant." "Cerebral edema (imaging diagnosis)" and "elevated intracranial pressure (ICP sensor)" merely look at intracranial pressure, which is the "result" of "secondary disorders" such as cerebral ischemia, hypoxia, status epilepticus, CSD (cortical spreading depolarization), and neuronal cell death. In randomized controlled trials (RCTs) over the past 10 years, "ICP-based treatment" has been rated poorly, while "prevention" of ICP elevation by treating "secondary disorders" early after injury has been rated well. Since there is no equipment at the bedside to quickly diagnose "secondary disorders," neurointensivists (neurosurgeons, emergency physicians, and intensive care physicians) treat patients by "rules of thumb" until changes are seen on images or ICP sensors. As a result, patients die or become bedridden due to increased brain pressure or cerebral edema, and the prognosis does not improve.
Based on the consensus that "multimodal neuromonitoring" should provide neurointensivists with continuous and real-time neurophysiological information to prevent, detect and mitigate secondary injuries and improve prognosis, we have developed a safe, real-time bedside diagnostic system to rapidly diagnose and treat secondary injuries and improve the prognosis of severe brain injuries. This sensor definitely meets the "unmet medical needs". Since cerebral edema caused by secondary injuries peaks within 24-48 hours, there is a sufficient time window to use this system for effective diagnostic and therapeutic intervention.
In recent years, non-invasive or minimally invasive diagnostic devices have become popular around the world, but the only way to measure ICP, the gold standard for diagnosing severe brain injuries, is to invasively insert a sensor into the skull. When invasiveness is essential, our multifunctional sensor with a wide variety of parameters is the best choice. In addition, new AI diagnoses and treatments using digital data from the brain are being attempted, and this device, which can simultaneously obtain multi-element data, is the best match.
Future perspective